Anti-Epileptic Drugs in Pregnancy: What Every Woman Needs to Know
Understanding the Risks: AEDs and Pregnancy
If you are a woman of childbearing age taking anti-epileptic drugs (AEDs), it’s vital to know how these medications may affect your pregnancy and the developing baby. At INFACT, we support and advocate for women and families impacted by prenatal exposure to anti-seizure medications. This page provides clear, evidence-based guidance to help you make informed choices and feel empowered when speaking to your healthcare team.
Many epilepsy medicines carry risks during pregnancy, some more serious than others. Certain AEDs have been linked to birth defects, developmental delays, learning difficulties, autism spectrum conditions, and other long-term health problems in babies exposed in the womb.
Our Reach: Supporting Women Taking AEDs
We are here for you. Whether you are planning a pregnancy, currently pregnant, or taking medication for epilepsy or other conditions like migraines, mood disorders, or neuropathic pain, we want to ensure you have the information, guidance, and support you need.
This page covers the current known risks of AEDs in pregnancy, including those used not just for epilepsy, but also for pain, anxiety, bipolar disorder, and more. We urge all women to speak to their GP, neurologist, or epilepsy specialist before stopping or changing any medication.
“Epilepsy Medication Pregnancy Risks: What Every Woman Should Know”
Below is an overview of the most commonly prescribed AEDs and the risks they may pose during pregnancy, based on available safety warnings, research, and guidance from regulators such as the MHRA and EMA.
⚠️ High-Risk AEDs – Known to Cause Birth Defects or Neurodevelopmental Disorders
These medicines are associated with a significantly increased risk of harm to the unborn baby:
Valproic Acid / Sodium Valproate: Extremely High risk Associated with up to a 40% risk of developmental disorders and a 10% risk of birth defects. Should never be used in pregnancy unless no suitable alternatives exist.
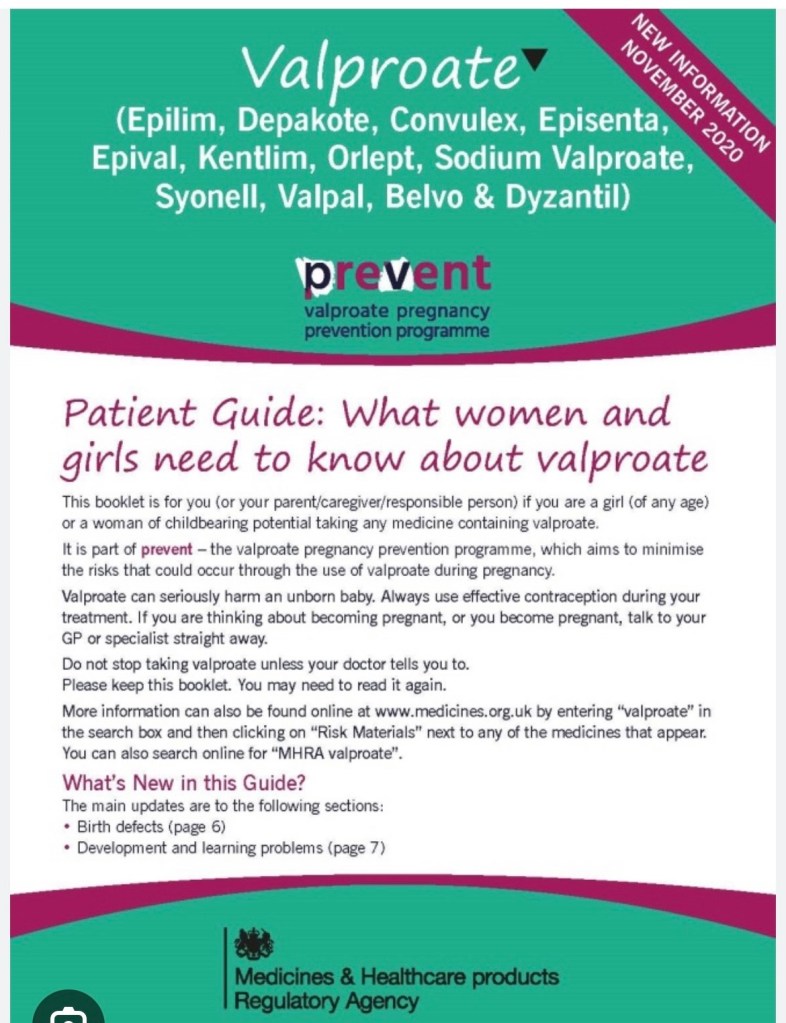
A strict Pregnancy Prevention Programme is in place.
Topiramate – Extremely High Risk Topiramate can harm an unborn child. If you are a woman who is able to become pregnant, talk to your doctor about other possible treatments. Visit your doctor to review your treatment and discuss the risks at least once a year.
• If you take Topiramate during pregnancy, your child has a higher risk for birth defects. In women who take topiramate, around 4 – 9 children in every 100 will have birth defects. This compares to 1-3 children in every 100 born to women who do not have epilepsy and do not take an antiepileptic treatment. Particularly, cleft lip (split in the top lip) and cleft palate (split in the roof of the mouth) have been observed. Newborn boys may also have a malformation of the penis (hypospadia). These defects can develop early in pregnancy, even before you know you are pregnant. • If you take Topiramate during pregnancy, your child may have a 2- to 3-fold higher risk for autism spectrum disorders, intellectual disabilities, or attention deficit hyperactivity disorder (ADHD) compared with children born to women with epilepsy not taking antiepileptic medication. • If you take Topiramate during pregnancy, your child may be smaller and weigh less than expected at birth. In one study, around 18 in every 100 children of mothers taking topiramate during pregnancy were smaller and weighed less than expected at birth, while around 5 in every 100 children born to women without epilepsy and not taking antiepileptic medication were smaller and weighed less than expected at birth. • Talk to your doctor if you have questions about this risk during pregnancy. • There may be other medicines to treat your condition that have a lower risk of birth defects.
A strict Pregnancy Prevention Programme is in place
Phenobarbital – Phenobarbital therapy in epileptic pregnant women presents a risk to the foetus in terms of major and minor congenital defects including congenital craniofacial and cardiac defects, digital abnormalities and, less commonly, cleft lip and palate. Studies in women with epilepsy who were exposed to phenobarbital during pregnancy identified a frequency of major malformations of 6-7% in their offspring compared to the background rate in the general population of 2-3%. Studies have found the risk of congenital malformations following in-utero exposure to phenobarbital to be dose dependent, however, no dose has been found to be without risk. Therefore, the lowest effective dose should be used
Phenytoin – Taking phenytoin during pregnancy increases the chance that the baby may have a physical birth abnormality. Studies with women treated with phenytoin for epilepsy during pregnancy have shown that around 6 babies in every 100 will have serious physical birth abnormalities. This compares to 2-3 babies in every 100 born to women who don’t have epilepsy. The most common types of serious physical birth abnormalities (major congenital malformations) reported for phenytoin include abnormalities of the lip and palate, heart, skull, nail and finger disorders and growth abnormalities. Some of these may occur together as part of a foetal hydantoin syndrome.
Primidone – If taken during pregnancy, Primidone which is extensively metabolised to phenobarbital can cause serious birth defects and can affect the way in which the child develops as it grows. Birth defects which have been reported in studies include cleft lip (split in the top lip), cleft palate (split in the roof of the mouth) and heart abnormalities. Other birth defects have also been reported, such as malformation of the penis (hypospadias), smaller than normal head size, facial, nail and finger abnormalities. If you take phenobarbital during pregnancy you have a higher risk than other women of having a child with birth defects that require medical treatment. In the general population, the baseline risk of major malformations is 2-3%. This risk is increased by about 3 times in women taking phenobarbital (main metabolite of primidone). Primidone should not be used during pregnancy unless nothing else works for you.
Carbamazepine – Taking carbamazepine during pregnancy increases the chance that the baby may have a physical birth abnormality (major congenital malformations). Studies with women treated with carbamazepine for epilepsy have shown that on average 4-5 babies in every 100 will have serious physical birth abnormalities. This is compared with 2 to 3 babies in every 100 born to women who do not have epilepsy. These abnormalities can develop early in pregnancy, even before you know you are pregnant. The most common types of major congenital malformations reported for carbamazepine include spina bifida (where the bones of the spine are not properly developed); facial and skull malformations including cleft lip/palate; skeletal, heart, urinary tract and sexual organ malformations.
These medications may increase the risk of spina bifida, cleft palate, heart defects, and problems with cognitive development. Alternative treatment options should always be discussed with a specialist.

Birth Defects Linked to Epilepsy Medicines
⚠️ Medications Requiring Caution – Potential Risks, More Research Needed
These drugs have shown some signals of potential harm, but data is either limited or varies across studies. Caution and close medical oversight are essential:
Pregabalin – Lyrica should not be taken during pregnancy or when breast-feeding, unless you are told otherwise by your doctor. Pregabalin use during the first 3 months of pregnancy may cause birth defects in the unborn child that require medical treatment. In a study reviewing data from women in Nordic countries who took pregabalin in the first 3 months of pregnancy, 6 babies in every 100 had such birth defects. This compares to 4 babies in every 100 born to women not treated with pregabalin in the Page 4 of 8 study. Abnormalities of the face (orofacial clefts), the eyes, the nervous system (including the brain),kidneys and genitals have been reported
Gabapentin – Gabapentin capsules can be used during the first trimester of pregnancy if needed. If you plan to become pregnant or if you are pregnant or think you may be pregnant, talk to your doctor straight away. If you have become pregnant and you have epilepsy, it is important that you do not stop taking your medicine without rst consulting your doctor, as this may worsen your illness. Worsening of your epilepsy may put you and your unborn child at risk. In a study reviewing data from women in Nordic countries who took gabapentin in the rst 3 months of pregnancy, there was no increased risk of birth defects or problems with the development of brain function (neurodevelopment disorders). However, babies of women who took gabapentin during pregnancy had an increased risk of low birth weight and preterm birth. If used during pregnancy, gabapentin may lead to withdrawal symptoms in newborn infants. This risk might be increased when gabapentin is taken together with opioid analgesics (drugs for treatment of severe pain). Contact your doctor immediately if you become pregnant, think you might be pregnant or are planning to become pregnant while taking Gabapentin capsules. Do not suddenly discontinue taking this medicine as this may lead to a breakthrough seizure, which could have serious consequences for you and your baby.
Lamotrigine – Considered lower risk but may still carry a small increase in cleft palate risk. Must be closely monitored. Studies of women who took lamotrigine at usual doses while they were pregnant have not shown an increased risk of physical birth abnormalities. • The risk of physical birth abnormalities may increase when higher doses of epilepsy medicines are taken or more than one epilepsy medicine is used at the same time. Where possible, your doctor will consider using one epilepsy medicine at the lowest effective dose to control your epilepsy • There may be a small increased risk of birth defects, including a cleft lip or cleft palate, if Lamotrigine is taken during the first 3 months of pregnancy.
Levetiracetam – Levetiracetam can be used during pregnancy, only if after careful assessment it is considered necessary by your doctor. You should not stop your treatment without discussing this with your doctor. A risk of birth defects for your unborn child cannot be completely excluded. Breast-feeding is not recommended during treatment.
Oxcarbazepine – Neurodevelopmental disorders – Some studies have shown that exposure to oxcarbazepine in the womb negatively affects the development of brain function (neurodevelopment) in children, while other studies have not found such an effect. The possibility of an effect on neurodevelopment cannot be ruled out. Your doctor will tell you the benefits and potential risks involved and help you to decide whether you should take Trileptal. Do not stop your treatment with Trileptal during pregnancy without first checking with your doctor
Zonisamide – Studies have shown an increased risk of physical birth abnormalities in children of women taking epilepsy medicines during pregnancy. The risk of physical birth abnormalities may increase when more than one epilepsy medicine is used at the same time. Where possible, your doctor should consider using one epilepsy medicine to control your epilepsy. More research is needed to better understand whether taking zonisamide during pregnancy increases the risk of having a baby born with a physical birth abnormality or a learning or thinking disability. Studies have shown that babies born to mothers using zonisamide during pregnancy were smaller than expected for their age at birth, compared with babies born to mothers treated with lamotrigine monotherapy.
Lacosamide It is not recommended to take Lacosamide if you are pregnant, as the effects of lacosamide on pregnancy and the unborn baby are not known. It is not recommended to breast-feed your baby while taking lacosamide, as lacosamide passes into breast milk. Seek advice immediately from your doctor if you get pregnant or are planning to become pregnant. They will help you decide if you should take Lacosamide or not. Do not stop treatment without talking to your doctor first as this could increase your fits (seizures). A worsening of your disease can also harm your baby.
Brivaracetam – If you are pregnant or breast-feeding, think you may be pregnant or planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine. It is not recommended to take Briviact if you are pregnant, as the effects of Briviact on pregnancy and the unborn baby are not known. It is not recommended to breast-feed your baby while taking Briviact, as Briviact passes into breast milk. Do not stop treatment without talking to your doctor first. Stopping treatment could increase your seizures and harm your baby.
Clobazam A large amount of data has not shown evidence for malformations associated with the use of benzodiazepines. However, some studies have shown a potentially increased risk of cleft lip and palate in newborn babies compared to that in the general population. Cleft lip and palate (sometimes called ‘harelip’) is a deformation at birth caused by incomplete fusion of the palate and upper lip. Reduced fetal movement and fetal heart rate variability may occur after taking clobazam during the second and/or third trimester of pregnancy. If Clobazam is taken at the end of pregnancy or during childbirth, your baby may show drowsiness (sedation), muscle weakness (hypotonia or floppy infant syndrome), a drop in body temperature (hypothermia), difficulty feeding (problems suckling causing poor weight gain) and breathing problems (respiratory depression, sometimes severe). If taken regularly in late pregnancy, your baby may get withdrawal symptoms such as agitation or shaking. In this case the newborn should be closely monitored during the postnatal period. Do not take Clobazam if you are breast-feeding or are planning to breast-feed. This is because it may pass into the mothers’ milk
Clonazepam – Do not take Clonazepam Neuraxpharm if you are pregnant, might become pregnant or are breast[1]feeding, unless your doctor tells you to. Clonazepam is known to have harmful effects on the unborn child.
Perampanel – Perampanel Eisai is not recommended in pregnancy. – You must use a reliable method of contraception to avoid becoming pregnant while you are being treated with Perampanel Eisai. You should continue doing this for one month after stopping treatment. Tell your doctor if you are taking hormonal contraceptives. Perampanel Eisai may make certain hormonal contraceptives such as levonorgestrel less effective. You should use other forms of safe and effective contraception (such as a condom or coil) when taking Perampanel Eisai. You should also do this for one month after stopping treatment. Discuss with your doctor what may be appropriate contraception for you
Rufinamide – If you are pregnant, or think you might be pregnant, or are planning to get pregnant, ask the doctor or pharmacist for advice before taking Rufinamide Eisai. You must only take Rufinamide Eisai during your pregnancy if the doctor tells you to. You are advised not to breast-feed while taking Rufinamide Eisai, as it is not known if rufinamide will be present in breast milk. 3 If you are a woman of childbearing age, you must use contraceptive measures while taking Rufinamide Eisai. Ask the doctor or pharmacist for advice before taking any medicine at the same time as Rufinamide Eisai.
Tiagabine – As a precautionary measure it is NOT advised to take Gabitril during pregnancy or breastfeeding
Stiripentol – If your child is pregnant or breast-feeding, think she may be pregnant or is planning to have a baby, ask your doctor for advice before taking this medicine. During pregnancy, effective epilepsy treatment must NOT be stopped. Breast-feeding is not recommended during treatment with this medicine
Cenobamate – If you are pregnant or breast-feeding, think you may be pregnant, or are planning to have a baby, ask your doctor or pharmacist for advice before you take this medicine. Only take Ontozry during pregnancy if you and your doctor decide that it is absolutely necessary. You must use effective contraception during use of cenobamate and until 4 weeks after you stop taking this medicine. Ask your doctor for advice regarding effective measures of birth control. You should stop breast-feeding while taking Ontozry.
Eslicarbazepine Acetate – There are no data from the use of eslicarbazepine acetate in pregnant women. Research has shown an increased risk of birth defects in children of women taking antiepileptic medicines. On the other hand effective antiepileptic therapy must not be interrupted since the worsening of the disease is harmful to both the mother and the unborn child. Do not breast-feed while you are taking Eslicarbazepine Zentiva. It is not known whether it passes into breast milk
Vigabatrin – Do NOT take Sabril during pregnancy unless your Drs tell you too. Sabril may cause problems to unborn children. However do not stop taking this medication suddenly because this may risk the mothers health as well as the babies
Ethosuximide – In case you are able to get pregnant your doctor will advise you to plan and monitor your pregnancy before starting the treatment with Ethosuximide Strides. Do not suddenly stop using this medicine since it may lead to breakthrough seizures that could harm you or your unborn child. Tell your doctor immediately if you are pregnant, think you may be pregnant or are trying for a baby
Everolimus – Everolimus could harm your unborn baby and is not recommended during pregnancy. Tell your doctor if you are pregnant or think that you may be pregnant. Your doctor will discuss with you whether you should take this medicine during your pregnancy. Women who could potentially become pregnant should use highly effective contraception during treatment and for up to 8 weeks after ending treatment. If, despite these measures, you think you may have become pregnant, ask your doctor for advice before taking any more Everolimus.
Piracetam – If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine. If you are taking this medicine, use contraception to avoid becoming pregnant. If you are taking Nootropil Tablets and you think you may be pregnant, consult your doctor immediately.
Cannabidiol (CBD for epilepsy) – Limited human data; not enough evidence to confirm safety in pregnancy. If you are pregnant, think you may be pregnant, or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine. You should not take Epidyolex while you are pregnant unless the doctor decides the benefits outweigh the potential risks. You should not breast-feed whilst taking Epidyolex, as Epidyolex is likely to be present in breast milk.
Buccal Midazolam – If the patient who will be given this medicine is pregnant or breast-feeding, thinks she may be pregnant or is planning to have a baby, ask a doctor for advice before taking this medicine. Giving high doses of BUCCOLAM during the last 3 months of pregnancy can cause abnormal heart beat in the unborn child. Babies born after this medicine is administered during childbirth can also have poor suckling, breathing difficulties and poor muscle tone at birth.
Newer medicine; caution advised. If you or your child are pregnant, think you or your child might be pregnant, or are planning to have a baby or are breast-feeding, ask your doctor for advice before taking this medicine.
Know Your Rights – Get the Information You Deserve
If you’re taking any of these medications and are pregnant or planning a pregnancy, you have the right to:
- Be fully informed about the risks.
- Be offered a pre-conception consultation.
- Have your treatment reviewed by a specialist.
- Access the Pregnancy Prevention Programme (PPP), especially if you’re taking Valproate or Topiramate
Take Action Today: Steps to Protect Your Pregnancy
- Don’t stop taking your medication without medical advice.
- Speak to your neurologist or GP about your plans for pregnancy.
- Ask about safer alternatives.
- Request referral to a specialist if you haven’t already.
- Keep records of all consultations and medication changes.
We’re Here to Support You
At INFACT, we campaign for safer prescribing practices, informed consent, and proper regulation of high-risk medications in pregnancy. If you have concerns or need guidance, please reach out to us. You are not alone, and you deserve the truth, support, and the safest options possible.
Please join our online community support group

